Are you a member?
If you’re looking for more information about your pharmacy benefits or need to log in to the member portal, click below to visit our Members page.


We are a different kind of PBM.
We do not own pharmacies.
Alluma aligns incentives across your drug purchasing program, on-site pharmacies, clinical practice, employee health plans, and members, creating a cohesive strategy that maximizes value.


We partner with our clients to achieve the best outcomes.
We negotiate on the same side as our clients.
Alluma is a provider-led, provider-focused Pharmacy Benefits Manager (PBM) that prioritizes patient outcomes over profits. Alluma is committed to transparency, clinical collaboration, and resource optimization.

We are Pharmacy Benefit Illuminators
Transparency you can trust
See true net cost with no hidden margins and pricing not driven by utilization. Clear insights replace opaque PBM economics so you can make confident decisions.
Clinical collaboration that matters
Work directly with healthcare pharmacists and clinical experts who align benefit design with evidence-based care and real-world provider insight.
Insight that drives action
Real-time data and strategic guidance turn complexity into clarity, helping you uncover savings opportunities and improve pharmacy performance.
High-touch partnership
Dedicated account teams act as an extension of your organization, delivering proactive guidance and concierge-level support at every stage.
Why organizations choose Alluma
Alluma is more than a PBM. Our provider-led model gives organizations the clarity and expertise needed to make confident pharmacy benefit decisions that support both outcomes and long-term sustainability.
Organizations partner with Alluma to:
- Gain true cost transparency with clear visibility into net cost, no hidden margins and pricing that is not driven by utilization
- Collaborate clinically with healthcare pharmacists and care teams to align benefit design with evidence-based care
- Turn data into insight through real-time reporting and strategic guidance that informs smarter decisions
- Receive dedicated, high-touch support from experienced account teams that act as an extension of your organization, delivering proactive guidance and concierge-level service
- Strengthen performance and experience for members, patients and the organizations that serve them
Whether you are strengthening a health system pharmacy ecosystem or evolving pharmacy benefits for your workforce, Alluma delivers the insight, alignment and advocacy needed to achieve measurable results.
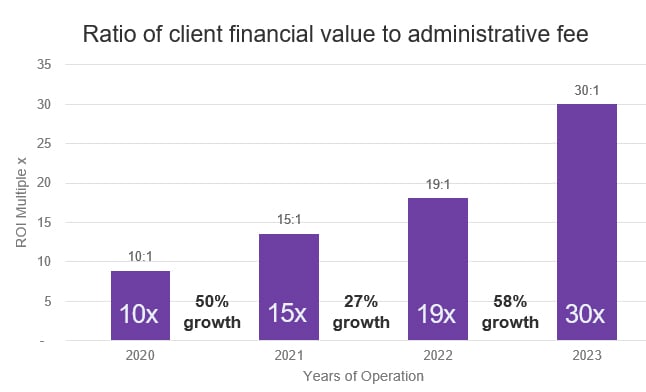
Alluma model continues to support client growth
100% pass-through of rebates and savings
- Alluma provides 100% pass-through of rebates and savings: 30:1 return on admin fee in 2023
- Alluma drives significant volume to the on-site pharmacies of its health system clients: 20% higher fill rate on average compared to the market
- Alluma members have consistently shown 15% higher formulary compliance relative to the Employer-Hospital Benchmark, which contributes to above-market savings
- With the Alluma model, on average, 49% of claims were captured, equating to 51% of revenue
Stay informed
Sign up for email updates and get the latest news, industry trends and expert tips delivered straight to your inbox. Be the first to learn how we’re transforming pharmacy benefits and helping organizations like yours achieve better health outcomes.